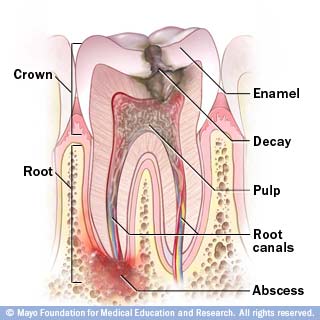
When a child receives a blow to the mouth and injures a front tooth, there is always a chance that the blood supply to the dental pulp (or nerve) will be severed, causing the nerve to die. In this case, root canal treatment would be indicated. However, if the child is of a younger elementary school age, the end of the root has probably not matured yet.
This is a situation called an open apex. The apex is the tip of a tooth root. In a normal root canal, an inert filling material is packed against the apex to seal the end of the root. With an open apex, there is nothing to pack against so there is no way to get a good seal. Fortunately, there is a procedure called apexification that will stimulate the body to close the apex. After the root canal has been thoroughly cleansed of debris, a calcium hydroxide paste is inserted at the root end. The calcium hydroxide is very alkaline. The body reacts to this high pH by depositing hydroxylapatite crystals (the basic building blocks of teeth) at the site. It takes a few visits spaced out over a year’s time and then the canal can be properly sealed. Using this procedure will allow a front tooth to be retained, saving the child from years of embarrassment and numerous tooth replacements.